The objective of this fully accredited ACGME-approved AP/CP training program is to produce leaders in diagnostic pathology and biomedical research.

Specific educational goals and objectives are designed to ensure that each trainee acquires the body of knowledge, skills, attitudes and behaviors desirable in a modern, world class pathologist.
Frequently Asked Questions
Why Duke Pathology?
We have a decades-long track record of being a top-tier program that graduates outstanding pathologists who excel in academic, community, and industry settings. Our faculty are committed to excellence in patient care, education, and research, and our program provides numerous career opportunities. Duke Hospital is situated on the beautiful campus of Duke University that houses the undergraduate and graduate schools. Durham is a thriving city that is a great place to live, work, and play; offers myriad social, entertainment, and athletic events; is situated within 2-3 hours of the coast and the mountains; and benefits from a beautiful climate. Our residents and fellows love their program, and are proud to be Blue Devils! Learn more about life in Durham.
Are surgical pathology rotations on a 1-day cycle?
Yes! A typical day involves the following activities: After morning conference, residents sign out with faculty; after sign out they gross their cases; and, then they preview cases for the next morning’s sign out.
Are Anatomic Pathology (AP) and Clinical Pathology (CP) rotations integrated?
Yes! All four years are integrated. PGY-1 year includes three months of autopsy, six months of surgical pathology, and three months of CP rotations (includes one month of transfusion medicine, one month of microbiology, and one month of either chemistry, hematopathology, or molecular pathology).
Does the program support flexibility in scheduling to support career/fellowship exploration?
Yes! Residents work with the chief residents during preparation of the annual schedules.
Are there opportunities to teach medical students?
Yes! All residents are required to teach each year during the Duke School of Medicine MS1 Pathology course.
Are professional development opportunities available to residents?
Yes! Please visit the Duke Graduate Medical Education website for information: Unique Opportunities for Trainees | Duke Health GME
Is there a formal mentoring program?
Yes! PGY-1’s are paired with a faculty mentor and senior resident buddy.
Do residents have their own desks and microscopes?
Yes! All residents have a desk, a microscope, and a laptop. The resident rooms have windows. There is a stand-up desk option with a microscope and computer.
AP/CP Clinical Track
Combined Anatomic and Clinical Pathology, Clinical Track
A 48-month curriculum with 4 months of electives.
AP Requirements
- Surgical Pathology: 15 months
- Autopsy: 3 months
- Forensics, OCME: 1 month
- Cytopathology: 3 months
- Dermatopathology: 2 months
- Neuropathology: 1 month
Total AP Requirements: 25 months
AP conference topics
- Cytopathology
- Forensic and autopsy pathology
- Frozen sections
- Medical kidney pathology
- Surgical pathology lectures with paired slide and gross conferences:
- Bone and soft tissue pathology
- Breast pathology
- Dermatopathology
- Endocrine pathology
- Gastrointestinal pathology
- Genitourinary pathology
- Gynecologic pathology
- Head and neck pathology
- Hematopathology
- Liver pathology
- Neuropathology
- Ophthalmic Pathology
- Thoracic pathology
- Transplant pathology
- Unknown slide conferences
CP Requirements
- Clinical Chemistry and toxicology: 1 month
- Coagulation, Basic and Advanced: 1 month
- Cytogenetics: 1 month
- Laboratory Hematology and Hematopathology: 1 month
- *Hematopathology (including Flow Cytometry): 3 months
- *Liver Pathology: 1 month
- *Medical Kidney and Transplant Pathology: 1 month
- Microbiology: 2 months
- *Molecular Pathology: 1 month
- *Molecular Diagnosis Integration: 1 month
- Transfusion Medicine: 2 months
- Senior Rotations**: 4 months (PGY 3 or 4)
Total CP Requirements: 19 months
CP conference topics
- AI and Informatics
- Clinical chemistry
- Coagulation
- Hematopathology
- Immunology
- Lab management
- Microbiology
- Molecular and cytogenetics
- Transfusion and apheresis
*Includes AP/CP variable rotations counted as CP rotations = 7
**Senior CP Rotations (PGY 3 and 4) = 4 months, chosen from the following three groups:
a. Competencies for Medical Directorship of Diagnostic Laboratory
| Medical Informatics | 1m | DUMC |
| Laboratory management project | 1m | VA/DUMC |
| Quality assurance project | 1m | VA/DUMC |
b. Molecular Pathology and Emerging Diagnostic Technologies
| Molecular Diagnostics-project | 1m | DUMC |
| Proteomics/Genomics/ FISH | 1m | DUMC |
c. Diagnostic Correlations and Consultations
| Transfusion /Coagulation Correlation | 1m | VA |
| Flow/Cytogenetics Correlation | 1m | DUMC |
d. Foundation Medicine Molecular Pathology elective rotation: Residents can choose to spend elective time as PGY-3 and/or PGY-4 at Foundation Medicine for a Molecular Pathology rotation at the Foundation Research Triangle Park laboratory campus.
During PGY2, 3 and 4, residents will select a clinical laboratory and participate as a “lab management apprentice” under the mentorship of the laboratory Medical Director.
Electives: 4 months
Electives may be selected from any of the required AP or CP rotations during PGY4. Other approved electives include: Autopsy, Cardiovascular Pathology, Cytogenetics, Electron Microscopy, Foundation Medicine Molecular Pathology, Gynecologic Pathology, Pulmonary Pathology, and Senior Microbiology (DUMC). Novel electives can be proposed and tailored to specific academic interests.
Summary
- AP = 25 months (American Board of Pathology requires 18)
- CP = 19* months (American Board of Pathology requires 18) [*includes AP/CP variable rotations counted as CP rotations = 7]
- Electives = 4 months
AP-only and AP/NP residency tracks are available for residents who enter the Physician-Scientist Research Pathway track.
We are pleased to offer one AP/NP position in ERAS NRMP for the 2025 Match.
Surgical Pathology Overview

A mastery over surgical pathology is a foundational skill required to successfully practice diagnostic pathology. Developing surgical pathology expertise is a slow process encompassing visual pattern recognition based on a vast body of medical knowledge and increasingly an integration with data derived from various ancillary molecular and other techniques. Recognizing the central role of these skills in our residents’ training, Duke Pathology training emphasizes Anatomic Pathology (Surgical Pathology and Autopsy Pathology) during the first year of residency, allowing the maximum period for “maturation”. In the initial year of training, each resident spends at least nine months on Anatomic Pathology services, with three autopsy months and six surgical pathology months. Three months of clinical pathology are also introduced. Subsequently, three months per year are devoted to surgical pathology with increasing responsibilities every year.
Typically three first year and three senior residents are on surgical pathology rotation at Duke. First year residents begin with a carefully graduated experience in the gross room, including detailed instruction in laboratory protocols and procedures for both large and small specimens. Residents then rotate in 2 week blocks on one of eight services: Gastrointestinal pathology, Gynecologic pathology, Bone and Soft Tissue pathology, Thoracic pathology, Breast pathology, Genitourinary pathology, ENT/endocrine pathology, and Frozen Sections/intraoperative consultations. Additionally, during years 2-4, residents rotate through dedicated subspecialty services in Dermatopathology, Cytopathology/FNA, and Neuropathology. Forensic Pathology training is gained through a one month rotation at the North Carolina Chief Medical Examiner’s office in Raleigh, N.C.
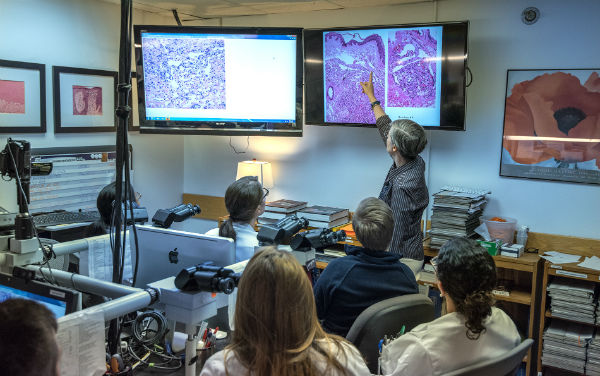
Attending faculty members rotate on a similar weekly schedule to assure a close working relationship with housestaff. Residents are given graded responsibility appropriate for level of training. Several modern multiheaded microscopes and ample reference material are available which allows self-study as well as peer to peer teaching. Grossing of specimens takes place after morning sign-out, followed by preview of cases in preparation for sign-out the following morning with attending faculty. Senior level residents function at the level of a surgical pathology fellow with responsibilities including oversight of grossing by junior level residents, working with laboratory staff to establish appropriate work flow levels in the lab, “hot-seat” diagnostic decision making responsibility for frozen sections, and microscopic sign-out of cases with the attending.
The department is committed to quality patient care through rapid turnaround time as well as to superior resident education. These competing goals are achieved by expanding the role of Pathology Assistants in the gross room. Six Pathology Assistants are available to guide the residents through the initial learning process and to perform grossing of “routine” cases. The grossing and frozen section experience is augmented by laboratory technicians to assist with small biopsies and operating room courier duties. The histology laboratory in the Duke Clinical Labs operates 24 hours a day, assuring that slides are ready for resident preview early in the day.
The training program is characterized by direct and continuous interaction of residents, fellows, faculty members and pathology assistants. We have a high volume of excellent clinical and laboratory materials received as a result of Duke's nationally and internationally renowned departments of medicine and surgery. We are proud of the residents and fellows who train here and continue to be energized each year by their quality and character.


