Leveraging AI to Transform Pathology

Artificial Intelligence (AI) is set to advance the field of pathology, fundamentally changing how diseases are understood, diagnosed, and treated. At the forefront of this transformation is Duke's Department of Pathology, in collaboration with Duke Artificial Intelligence (AI) Health. Together, they have established Duke’s Artificial Intelligence and Computational Pathology Division, a pioneering initiative aimed at enhancing the accuracy, efficiency, and predictive power of diagnostic practices. This advancement hopes to provide quicker, more accurate diagnoses that can lead to earlier, life-saving interventions for patients and their loved ones.
The Department has identified priorities and started strategizing investments that will allow for the deployment of digital pathology and computational image analysis into the clinical service. The goal is to further improve diagnostic accuracy, prognostication, prediction, and ultimately personalized treatment. These advancements are designed to provide patients with treatments specifically tailored to their unique medical needs, improving outcomes and reducing the uncertainty that often accompanies medical care.
Digital Pathology
Duke has made strategic investments in digital pathology, progressing from analog to digital imaging and laying the foundation for innovative uses of AI in the future. Digital pathology involves the acquisition, management, sharing, and interpretation of pathology information in a digital environment. The cornerstone of making a diagnosis is often the glass slide, which contains very thin slices of stained tissue that pathologists visualize under a microscope. Now, the glass slides are being systematically scanned into whole slide images, which can be viewed on a computer monitor or mobile device, enabling the "anytime, anywhere" model.
This digital infrastructure allows for the deployment of advanced methodologies, such as computational image analysis, which revolutionizes the way tissue damage is examined, quantified, and diagnosed. However, this requires a tremendous amount of investment in hardware, software, human intervention, and expertise necessary for implementation. Within the clinical labs, “We have been thoughtful in our approach,” commented Associate Professor of Pathology Diana Cardona, MD, “growing our capabilities by leveraging immediate gains in efficiency and cost effectiveness followed by the need for remote access and flexibility during the pandemic.” These initial efforts are increasing the lab’s and pathologists’ comfort level with this shift in practice, resulting in a growing demand and interest in asking the fun question of “what next?”
Computational Image Analysis
Digital pathology plays a pivotal role in computational image analysis, allowing for the implementation of AI algorithms to detect subtle patterns in both neoplastic and non-neoplastic diseases to improve diagnostic accuracy. AI excels in detecting "gaps"—subtle patterns or inconsistencies which can be overlooked by the human eye. These gaps can indicate early signs of disease or areas that require further investigation, making AI an invaluable tool for improving diagnostic sensitivity. By catching these early-warning signs, AI may help doctors intervene sooner, giving patients a better chance at successful treatment and recovery.
Leading the charge with AI and digital image analysis are co-directors of the Duke’s AI and Computational Pathology division, Carolyn Glass, MD, PhD, associate professor of Pathology, and Laura Barisoni, MD, professor of Pathology and Medicine. Several projects are conducted within the division. For example, Glass and Roarke Horstmeyer, PhD, assistant professor in Biomedical Engineering, are developing a digital polarization tool for remote diagnosis to enhance the accuracy and accessibility of specimen analysis. Meanwhile, Barisoni, Kyle Lafata, PhD, assistant professor of Radiation Oncology, and others have developed a workflow for the accurate and semi-automated assessment of kidney biopsies, which has potential to change current practices and provide patients with more precise and actionable diagnoses.
Using AI to identify intestinal metaplasia

Currently, Duke is working on a project to recognize precancerous changes in the stomach lining, specifically focusing on a condition known as intestinal metaplasia. This condition involves the transformation of the stomach lining to resemble the intestines, which can increase the risk of developing gastric cancer. By leveraging AI, the project aims to enhance the early detection and accurate diagnosis of intestinal metaplasia, ultimately improving patient outcomes through timely interventions. Although this is in initial testing, AI has already detected about 5% of cases that pathologists missed. While AI can make mistakes, these occur less frequently than human error. As William "Will" Jeck, MD, director of Digital Pathology and Enhanced Diagnostics, noted, “The real potential lies in the collaboration between AI and pathologists."
Jeck also co-leads the Nference project, which aims to scan nine million slides of Duke’s pathology archive. The project’s current research focuses on the development of practical implementation of AI and machine learning tools in pathology practice, supporting both diagnostic work and broader research efforts across the department. These initiatives are crucial to ensuring that AI and digital pathology enhance clinical care while maintaining regulatory and safety standards.
By combining efforts, the accuracy of diagnoses can be significantly enhanced, leading to more precise treatment plans and better outcomes for patients, ultimately reducing the anxiety and uncertainty for both patients and their loved ones. This collaborative effort involves feeding large datasets into AI systems, which then learn to recognize subtle patterns indicative of disease. "It’s about giving the machine good data to work from and our ability to analyze the machine’s analysis," said Jeck. The insights gained from these computational models are helping to refine diagnostic criteria and treatment protocols, contributing to more precise and effective medical care. What this means for those newly diagnosed is hope. It means catching cancer earlier, when it is more treatable, offering a better prognosis and greater peace of mind.
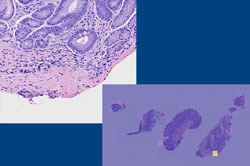
intestinal metaplasia (low-power image with AI overlay
on right) missed by the original signing pathologist and
three subsequent independent reviews, but agreed upon
following review of the AI results. AI offers a way to provide
quality control and improve diagnosis of focal findings.
Intestinal metaplasia can be a sign of other important
diseases, such as autoimmune gastritis or helicobacter
pylori infection. It is also a risk factor for gastric cancer.
Going beyond the human eye
Computational image analysis leverages AI to identify and quantify characteristics beyond the capabilities of human vision. This approach is being championed at Duke by experts, such as Lafata and Barisoni, who is an international leader in digital nephropathology. Barisoni's team, which includes biomedical and electrical engineers, physicists, and statisticians, uses AI to develop algorithms that accurately identify and classify kidney structures. They also apply pathomics—the study of tissue characteristics—to extract and quantify subvisual features, better characterizing kidney diseases and identifying digital biomarkers of disease progression. These technologies are currently being implemented in clinical research, with the goal of establishing robust AI-based protocols in clinical settings. The clinical deployment of these algorithms holds immense potential for improving pathologists' performance and enhancing patient care. These efforts have the potential to directly contribute to better treatment outcomes, giving patients access to cutting-edge diagnostics.
Predictive Analysis
Predictive analysis leverages AI to examine historical patient data, helping predict disease progression and outcomes. This is particularly useful for diseases like gastrointestinal (GI) and liver disorders, where early and accurate predictions can significantly impact treatment plans. By anticipating how a disease might progress, doctors can tailor treatment plans to each patient’s needs, providing a more personalized approach that could improve the chances of successful treatment.
Duke is using predictive analysis to enhance patient care by anticipating disease trajectories. AI can be attentive to every case and absorb vast amounts of data during its training, allowing it to see patterns across multiple institutions. "AI has the ability to ingest an immense amount of data, including information from multiple institutions; whereas we, humans, wouldn’t be able to analyze all of that on our own," said Jeck. This capability enables AI to provide insights that might be overlooked by human analysis alone, leading to more informed and proactive treatment decisions. For patients, this means they can benefit from more accurate predictions about their health, allowing them to plan and make decisions. This can result in more accurate and timely treatments, potentially saving lives by catching diseases before they progress.
The use of AI in predictive analysis at Duke is exemplified by ongoing research projects that aim to refine these predictive models further. By continuously feeding new data into these AI systems, researchers are improving the accuracy and reliability of disease progression forecasts, ultimately benefiting patient care.
Personalized Medicine

Traditional medicine often relies on analyzing data across large groups of patients in clinical trials to determine the best diagnostics, prognostics, and treatments. However, what is considered optimal care on average might not be the best approach for an individual patient. Personalized medicine focuses on tailoring medical care based on a patient's unique genetic and phenotypic characteristics. At Duke, efforts are underway to develop AI tools that can analyze these characteristics and predict how a patient's disease will progress and respond to different treatments.
Professor of Pathology Rajesh Dash, MD, chair of the College of American Pathologists (CAP) Artificial Intelligence Committee, is spearheading efforts to prepare pathologists nationwide for the transformative impact of AI on personalized diagnostics, prognostics, and treatment strategies. At Duke, Dash is part of a team prototyping real-time AI diagnostics during bronchoscopy procedures, where cytology specimens are collected. His collaborators include Kamran Mahmood, MD, MPH, a pulmonologist and associate professor of Medicine, as well as Glass and Horstmeyer.
The potential for AI to enhance access to personalized medicine is immense. This approach means that treatments can be tailored specifically to each patient's genetic makeup, improving the chances of a successful outcome and reducing the risk of adverse reactions. By integrating genetic, molecular, and clinical data, AI can help identify the most effective treatment plans for individual patients, minimizing trial-and-error in medical practice and improving overall outcomes.

Improving Diagnostic Accuracy
Computer-aided diagnostics have the potential to increase accuracy, prognostication, and predictive value above and beyond current practices. Danielle Elliott Range, MD, associate professor of Pathology and vice chair, medical director, and chief of Duke's Cytology Division, emphasizes the role of AI in advancing diagnostic accuracy in cytopathology. “Artificial intelligence has been integral to the clinical practice of cytopathology for decades. In combination with human expertise, AI is superior to either alone in diagnosing cervical lesions on Pap smears,” she said. “The use of AI in cytopathology will be key to improving diagnostics in other specimen types as well.” Advocating for the inclusion of diverse populations in AI research ensures that these technologies benefit all patients equitably.
Range is currently working on a project to design an algorithm that will assist pathologists in low-resource areas in the diagnosis and classification of thyroid tumors. By improving diagnostic accuracy in underserved areas, this project has the potential to significantly impact patient outcomes globally, offering hope to patients who might otherwise have limited access to advanced medical care. “Projects like these bring a level of medical expertise to remote parts of the world, significantly impacting global healthcare delivery,” she explained.
Clinical Deployment

Duke Pathology is at the cutting edge of integrating AI into medical practice, paving the way for groundbreaking advancements in disease diagnosis, treatment, and research. The collaborative efforts of Duke’s experts in digital image analysis, predictive analysis, personalized treatment, computational models, and diagnostic accuracy highlight the transformative potential of AI in pathology. As these technologies continue to evolve, there is a palpable excitement for the future, filled with hope for improved healthcare and support for clinicians facing the challenges of modern practice.
AI’s role at Duke includes ongoing training and validation of AI algorithms. These efforts are crucial for ensuring that AI tools meet rigorous clinical standards before widespread implementation. "It's a process to hand automation over. Right now, we are in the step in-between. We are teaching AI while still learning how best to do that," said Jeck. The integration of AI into diagnostic workflows promises to reduce human error, standardize diagnoses, and ultimately improve patient outcomes. For patients and their families, this means more accurate diagnoses, quicker treatment plans, and a greater chance of positive outcomes, reducing the emotional and physical toll of prolonged medical uncertainty.
“There is robust investment and tremendous excitement in the potential of AI,” Glass shared, “but we also need to give close attention to ethics, as responsible AI is not trivial and should be taken into consideration.” With the FDA entering into this space of regulating laboratory developed tests and AI, another consideration is if burden and cost increase, will patient access decrease? Cardona weighed in, “This is something we are closely monitoring, and we are advocating for what is best for our patients, as the goal should always be to keep our patients safe while being able to provide leading-edge, high-quality testing and diagnostic information in the least burdensome way.”
"AI will completely transform anatomic pathology; however, this transformation will probably take a very long time," said Jeck. In similar accord, Glass shared, “Although the development of AI algorithms has become more popularized throughout leading academic centers in the world, the validation and actual clinical implementation science side of the field still remains a challenge. It will take heavy investment to move it forward.”
Notable AI-Related Achievements at Duke

- Strategic Partnership with Microsoft: Duke University and Duke Health have entered a five-year strategic partnership with Microsoft to support AI applications in medicine. This collaboration aims to advance healthcare delivery, champion health equity, and pioneer advanced research.
- Duke AI Health Director Appointment: Michael Pencina, PhD, has been named Duke Health’s first Chief Data Scientist. This role is designed to create a strategic direction for AI and data science at Duke Health, emphasizing both academic and clinical missions.
- Inaugural Duke Symposium on Algorithmic Equity and Fairness in Health: Duke AI Health and the Duke University School of Nursing held the inaugural Duke Symposium on Algorithmic Equity and Fairness in Health, addressing algorithmic bias in healthcare and developing methods and interventions to promote equity in health and healthcare delivery.
- Deployment of AI Tool 'Copilot' for Microsoft 365: Duke Health has implemented 'Copilot' to enhance healthcare delivery. This AI tool is designed to integrate with Microsoft 365 to improve efficiency and patient care.
- Digital Pathology Initiative at Duke University: Duke's Department of Pathology has invested in a comprehensive digital pathology initiative to digitize all histopathology slides, allowing for AI-driven image analysis and improved diagnostic accuracy.
AI Publications by Duke’s Pathology Team
- Application of a Machine Learning Algorithm to Predict Malignancy in Thyroid Cytopathology: Led by Danielle Elliott Range, MD, this project is designed to assist pathologists in low-resource areas by using smartphone images of thyroid cytology specimens to classify thyroid nodules.
- Development of AI Tools for Kidney Disease: Laura Barisoni, MD, and her team have developed AI algorithms for the accurate and semi-automated assessment of kidney biopsies, which have the potential to revolutionize the diagnosis and management of kidney diseases.
- Algorithm for Thyroid Nodule Classification: Led by Danielle Elliott Range, MD, this project involves the application of a machine learning algorithm to predict malignancy in thyroid cytopathology. The tool assists pathologists in low-resource areas by using smartphone images to classify thyroid nodules.
- Digital Polarization Tool for Remote Diagnosis: Developed by Carolyn Glass, MD, PhD, this tool enhances the accuracy and accessibility of specimen analysis, particularly in remote settings.