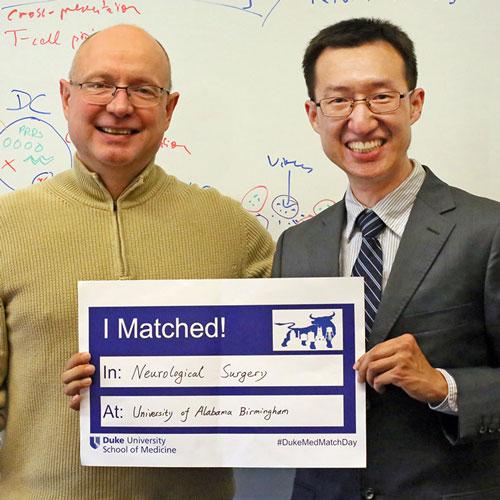
Yuanfan Yang, PhD Graduate student, matched into neurosurgery residency at the University of Alabama at Birmingham, which has a strong collaboration in neuro-oncology with Duke. Neurosurgery is one of the most competitive and difficult residencies to obtain, especially for foreign medical graduates.
Before coming to study brain tumor immunotherapy at Duke, Yang obtained medical training at Peking Union Medical College, founded by the Rockefeller foundation to modernize medical education in China, where he is originally from.
His grandfather was a Chinese engineer who serviced U.S. planes that delivered supplies to China in support of the combat against Japanese invasion during World War II. “When I went to college, he encouraged me to find where the need was the greatest, and to pursue that path for my community.” remembered Yang.
Structured neurosurgical residency training is not as established in China compared to the United States. Those interested in neurosurgery undergo apprenticeships with individual neurosurgeons on specific procedures, leaving gaps in training. One of the biggest gaps is to take care of children with neurological disorders. During medical school, Yang was selected by the China Medical Board for a neurosurgery clerkship at Harvard Medical School. This U.S. experience struck him deeply with its systematic training approach, ensuring exposure to diverse aspects of neurosurgery. His report on this experience was included in an effort to build a formal national neurosurgery residency in China. Although the proposal was placed on hold due to insufficient resources, he remained determined to become a neurosurgeon.
As a surgery trainee in China, he spearheaded a committee facilitating U.S. neurosurgery faculty to mentor and teach at a hospital in Beijing. They encouraged him to seek residency training in the U.S. and he decided to take the challenge.
“The field of neurosurgery also emphasizes scholarly work," noted Yang. "To better prepare myself, I pursued a PhD at Duke University after surgery residency. My project demanded delicate surgeries, to deliver an engineered poliovirus into tiny murine gliomas for microscopic analysis of the treatment response. After countless experiments refining my murine glioma workflow and careful observation of tumor pathology, I discovered a mechanism by which microglia mediate immune resistance to virotherapy. This finding supported a phase II clinical trial designed for polio virotherapy in recurrent glioblastoma (NCT04479241). The experience enhanced my confidence to thrive in such a discipline that demands precision, dexterity, and innovation. I was also fortunate to work with many faculty (especially Giselle Lopez, MD, PhD) who have recently gone through this process, and get their feedback on the trail,” said Yang. “That mentorship is critical for me to get into neurosurgery training in the United States."
“This is an especially great achievement as neurosurgery residencies are difficult to get into,” said Pathology Professor Soman Abraham, PhD. “Congratulations.”
