Cytopathology Fellow Alexandra “Tally” Balaban, MD, presented a poster titled “Distinguishing Non-Renal Cell Neoplasms on Kidney Fine Needle Biopsies” at the American Society of Cytopathology’s 72nd Annual Scientific Meeting in Orlando, Florida, from Nov. 6-10, 2024. Her co-authors were Hongzhi Xu MD, PhD, (previous Duke cytopathology fellow, now on the faculty at Moffitt Cancer Center), Ian Taylor-Cho, MD, (prior medical student at Duke, now a pathology resident at Stanford Medical Center), Xiaoyin (Sara) Jiang MD (current adjunct Duke faculty), and Duke Associate Professor of Pathology Wen-Chi Foo, MD.
Most lesions diagnosed through cytologic evaluation of renal mass fine needle biopsies (FNBs) are renal cell carcinomas (RCCs). Encountering non-renal-cell malignancies is rare and not widely studied in the context of cytology but has marked impact on subsequent treatment decisions.
A nine-year retrospective review (2015-2023) of renal mass FNBs was conducted at Duke University Medical Center. All patients with malignant renal masses evaluated by the Cytopathology Division but not diagnosed as RCC were included in the study. Patient demographics, imaging features, pathology, and clinical follow-up were collected.
Out of 370 renal mass biopsies, 53 (14.3%) were malignant, but not RCC. Most non-RCC malignancies were successfully diagnosed on renal cytology FNB. The diagnoses fell into one of six categories, including solid tumor metastasis (28%), carcinoma not otherwise specified (23%), lymphoma (21%), urothelial carcinoma (15%), sarcomatoid neoplasm (8%), and carcinoma with squamous differentiation (6%).
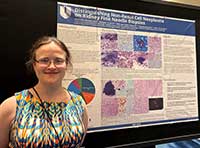
The most common metastatic tumor primary sites were head and neck, lung, and skin. Diagnostic challenges included scant viable tumor, loss of lineage defining markers in high-grade and/or sarcomatoid neoplasms, weak PAX8 expression in upper-tract urothelial carcinoma, and carcinoma with squamous differentiation. In cases with diagnostic uncertainty such as due to loss of lineage-defining markers, triaging material for molecular work-up proved invaluable. Challenges in rapid on-site evaluation (ROSE) diagnosis included recognizing lymphomas, abundant obscuring necrosis and scant viable tumor, non-exfoliating spindled tumors, and bland metastatic solid tumors.
With the results of this study, the authors hope to offer diagnostic insights and highlight pitfalls for cytologists, cytopathologists, and general practice pathologists when they are confronted with performing a ROSE or signing out a renal mass FNB case that falls outside the realm of primary RCC neoplasms.